GI Motility Testing: At a Glance
- Often the diagnosis of a functional GI disorder can be made with few or no tests.
- Sometimes tests are needed to rule out another disease.
- Usually some preparation is needed before the test may be done.
- Correct preparation for a test helps make it easier and more effective.
- Knowing what to expect will help you feel more at ease.
In many cases, doctors can make a diagnosis of a functional gastrointestinal disorder after a careful history and examination. Often, however, there is a structural disease that must be excluded by tests that probe the gastrointestinal tract.
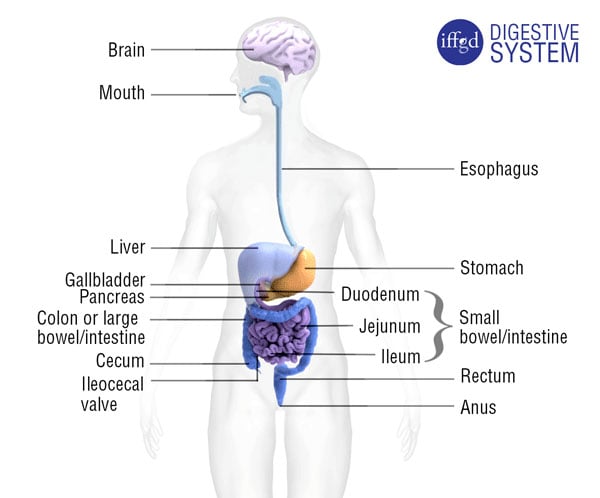
In dyspepsia, for example, upper abdominal distress may be due to a peptic ulcer in the stomach or duodenum, and an endoscopy may be required to rule out such lesions. In the case of irritable bowel syndrome (IBS) or constipation, there may be an alarm feature, such as blood in the stool or a family history of colorectal cancer that prompts a doctor to order a colonoscopy, sigmoidoscopy, or barium enema.
For these and other gastrointestinal investigations, some preparation is required. If you have to have one of these tests, it may help to know why the preparation is necessary and how to make it effective and less stressful.
General principles
When preparing yourself for an invasive gut procedure, it is well to keep in mind that the cleanliness and emptiness of the part to be examined is vital to success. If the examiner cannot see the colon wall because of a residue of stool, or the stomach because of a last-minute snack, there is a risk that he or she may fail to identify an important abnormality. Perforation of the colon is very rare, but will contaminate the abdominal cavity less if the organ is empty.
Often, during such a procedure, it is necessary to biopsy, cauterize, or remove a lesion, and that risks bleeding. It is therefore important to tell the doctors and nurses involved in the procedure what drugs you are taking, especially blood thinners (anticoagulants) and aspirin. The doctor may suspend these blood thinning drugs for the procedure. If your doctor agrees, aspirin (ASA, acetylsalicylic acid) should be stopped a week prior to the procedure in order to ensure that the blood platelets (small cells important in blood clotting) have returned to normal.
Iron may blacken the stool, reducing visibility. Therefore, iron-containing medication or diet supplements should be stopped 72 hours prior to a colonoscopy.
Sedation – Since some procedures require sedation, you must inform your doctor of any drug sensitivities, cardiovascular disease, or previous bad experiences with sedation. If sedation is to be given, or even possibly given, you should not drive from the clinic, but arrange to be picked up by a responsible party. Most facilities do not permit a cab trip home without a companion.
If you have diabetes, kidney failure, or other chronic disease, the doctor should be asked for special instructions regarding diet and medication.
There are many local variations in how, when, and what sedation is employed. For an endoscopy (a procedure that involves insertion, through the mouth or anus, of a thin, flexible tube used to look into the esophagus, stomach, duodenum, small intestine, colon, or rectum) an intravenous line usually is set up by the nurse after you arrive at the clinic.
The drugs are administered by injection into that line immediately before the test. There are many sedatives and relaxants available for this purpose. For the most part, the medications are safe and effective, but they require a period of recovery after their administration. You are not put to sleep since you need to be conscious and cooperative throughout. (This is called conscious sedation.) Tests of gut motility or function often require even more cooperation, and sedation is neither required nor advisable.
Sedation lessens any anxiety associated with the test. It may be given with a pain killer. The nurse or doctor will explain the possible adverse reactions particular to the drug or drugs used. Tolerances differ and too your reaction will be monitored. A device clipped to a finger permits the nurse to monitor your heart rate and blood oxygen saturation during the test.
The medications cause temporary forgetfulness; sometimes, examinees even forget having had the test. You may not even be able to remember or fully understand the test results if they are presented to you after the test. It is wise to arrange a follow-up meeting with the doctor to be sure that all the implications of these results are clearly addressed.
Local Anesthesia – Before starting a procedure that involves the insertion of an instrument into the esophagus and beyond, the nurse may apply a topical anesthetic to your throat. This is to help you swallow the instrument without gagging. The drug used is usually xylocaine and it may be applied as a spray, or as a gel that you swallow. It has a bad taste, and attempts to flavor it have had little success.
Consent – As with all medical procedures, you will be asked to sign a consent form that certifies that you understand the risks and benefits of the procedure, and that your doctor has explained them to you.
The consent procedure is an opportunity for you to ask questions. Normally, intestinal examinations are very safe. However, perforations of the organ may occur, especially when the area being examined is diseased, or if removal of a tissue sample (biopsy), cauterization, or removal of a polyp or foreign body is involved. This rare complication may require emergency surgery.
Before leaving the doctor’s office where the procedure has been arranged, be certain you understand everything about the procedure and its preparation. Failure to do this invites fear and misunderstanding, and it is often difficult and less satisfactory to correct these later by phone. As you sign the consent form you should understand with what, when, where, and why the procedure is being done, and if not satisfied, you should decline the test or seek a second opinion.
Sigmoidoscopy and colonoscopy tests
Sigmoidoscopy involves examination of the inside of the sigmoid colon and rectum using an endoscope. For a sigmoidoscopy, your doctor will instruct you to take a phosphate enema about 2 hours before the test. (However, in certain centers, a colonoscopy preparation (see below) is given in case a polyp is found that makes a colonoscopy necessary.) You should have only a light breakfast (or lunch) in the hours before the test. Some doctors use suppositories such as bisacodyl instead of an enema.
Colonoscopy is an endoscopic procedure in which the entire colon and rectum is viewed. If an abnormality is seen, it can be examined or removed. For a colonoscopy, it is imperative that the whole bowel be clean. The preparation must be thorough.
There are several methods, and your doctor must give you detailed instructions. You should plan to spend the preparation time with a toilet available nearby. The laxatives may be unpleasant, and sometimes they cause nausea and cramps. Nevertheless, they are safe when taken with clear fluids – and necessary if the examination is to be optimal. Adequate fluid intake should be maintained throughout. The product’s package insert will contain helpful advice on how to take the laxative(s). Elderly persons should be accompanied by a relative or friend when undergoing these preparations.
Other colonic procedures
A barium enema (barium allows the colon outline to be viewed on x-ray) requires preparation similar to that of a colonoscopy, but sedation is not required.
There are several other specialized and invasive tests of the colon such as colon or rectal manometry (measures sensation or contractions in the colon or rectum), balloon expulsion tests (measures ability to expel and retain stool), and defecography (looks at how well the rectum and anus work when defecating) that also need some preparation. However, these may differ from one diagnostic center to another.
Other than the discontinuation of drugs that affect the movements of the gut, no preparation is required for hydrogen breath testing, colonic scintigraphy, and radio-opaque marker studies of gut motility. Consult the articles listed below for more information regarding these procedures.
Upper gastrointestinal endoscopy
During an upper GI endoscopy the esophagus, stomach, and duodenum may be examined. The examiner will want your stomach empty during upper endoscopy. That’s the reason you will be instructed to fast. You should inform your doctor(s) if you are diabetic or are on important medication so that diet and medication can be planned.
When scheduling the test you should alert your doctor/endoscopist if you are taking anticoagulants or aspirin. These drugs increase the risk of bleeding if biopsy, cauterization, polyp removal, or esophageal dilatation is performed during the procedure. If your doctor agrees, aspirin should be stopped a week before. If you are to have sedation for the test you should arrange to have someone pick you up when you have recovered from the drug’s effects.
Other upper gut examinations
For radiological examinations of the esophagus, stomach, and duodenum, you are asked to swallow barium and x-rays are taken of the organs of interest. The preparation for this is similar to that of endoscopy, but anticoagulants need not be stopped, and no sedation is needed. Esophageal examinations such as esophageal manometry and a 24-hour pH probe (measures acid exposure in the esophagus) require an initial placement of a tube in the esophagus. Since that may cause retching, patients should be fasting.
However, the 24-hour pH probe measures the esophagus’s behavior during a normal day, so eating and other activities should be as normal as possible. Moreover, since drugs that affect esophageal motility may confound the results, they should be discontinued at least 24 hours before the procedure.
Summary
Many tests of the anatomy and function of the gastrointestinal tract require apparatus to be inserted through the mouth or anus. Where the gut interior is to be visualized by an endoscope or barium x-ray, a clean and empty interior is required if the examination is to be a success. In some tests of gut function, as little as possible should be done to interfere with the gut’s natural performance.
Sometimes fasting is necessary, but during such tests, eating and activity should be normal and drugs that might alter gut performance should be withdrawn. For detailed descriptions of these procedures, the reader is referred to the articles below.
More Resources
- Antroduodenal Manometry: Questions and Answers
- Colon Manometry
- Hydrogen Breath Tests
- Upper GI Endoscopy: What to Expect
- FAQs about Colonoscopies
- Tests for Chronic Constipation
- Diagnosis and Tests for GERD
- Diagnostic Tests in IBS Patients
- Testing of the Esophagus
- Testing of the Stomach
- Testing of the Small Intestine
- Testing of the Large Intestine
- Testing of the Anorectal and Pelvic Floor Area
